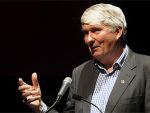
Looser criteria in the euthanasia law are needed, says ACT Party leader David Seymour.
A year after coming into force, the End of Life Choice Act is working well and opponents of the law change had “melted away,” Seymour says.
“The figures overwhelmingly show a law that is working. People can and do get through the process to become eligible for assisted dying, some change their mind, some are assessed as not eligible. That is what we’d expect if the law was working.”
In the year since the law was passed, 214 patients have been euthanased.
In all, 596 people have applied, and 294 have been deemed eligible and 120 people were turned down because they were not eligible.
Seymour says a third of the ineligible patients were declined because they didn’t meet the criteria of having a terminal illness likely to end their lives within six months.
He says he suspects “some if not many have an illness that is terminal but without a certain timeframe.”
Seymour says he agreed to the six-month timeframe to gain the Green Party’s support to pass the bill.
“I fear that compromise is leading to people … missing out on having choice and control, even though their long suffering is just as real as those with a more immediate terminal condition.”
His original bill would have allowed non-terminal patients with “grievous and irremediable conditions” to get access to voluntary euthanasia.
The amended law, which was voted on in a public referendum, made it explicit that applicants could not get access to assisted dying on the basis of disability or mental illness alone.
Seymour says he will argue for the euthanasia law criteria to be broadened when the law comes up for review in 2024.
He is also concerned that one in six applicants had died of underlying conditions before they were able to get an assisted death.
“It’s excluding people with long-term conditions, and that means a lot of suffering that may not be necessary,” he says.
Better palliative care
While Seymour wants the law relaxed, health experts are calling for wider support for palliative care services.
Royal College of GPs says it’s too early for any new legislation changes.
The College is calling for ongoing observation for the next 12 months.
The Royal College of GPs medical director, Dr Bryan Betty says he’d like more funding for palliative care services sector-wide.
“There is underfunding for hospice, there is underfunding for specialist palliative care services, and there’s under-funding of palliative care to general practices which support patients who are dying.”
Since December 2021, numbers seeking end-of-life treatment have risen from around 15 per month to around 20 in September 2022.
Source
Additional readingNews category: New Zealand.