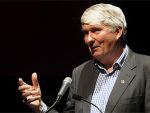
More palliative care investment is needed in New Zealand, says Royal College of GPs medical director Dr Bryan Betty.
He’s concerned about ACT Party leader David Seymour’s desire to widen the End of Life Choice Act criteria. Seymour argues the change is necessary, as many who want assisted suicide are “missing out”.
Seymour says this is mainly because those people don’t have a terminal illness likely to end their lives within six months.
The six-month terminal prognosis requirement prevents those with chronic conditions or disabilities from being eligible.
Betty argues broadening the eligibility criteria would not improve equitable choice for those facing end-of-life decisions.
It should not progress in light of the current palliative care climate in New Zealand, he cautions.
Nor should it happen without careful analysis.
Despite its supreme importance to New Zealand’s health system, palliative care is not well catered for, says Betty.
“There’s no strategic plan as to what is going to happen with palliative care, there’s fragmented services, lack of funding… the list goes on. It’s not a situation we can allow as a first-world, caring society.”
The contrast and imbalance of palliative care vs assisted suicide and euthanasia is sizeable and cause for concern, he says.
“We have one part of the system fully-funded and overseen in an apparently coherent way by the Ministry of Health (assisted suicide and euthanasia), and the other sector that doesn’t even have a strategic plan in place, that is inequitably funded, and has no coherent overview of how to develop the service.
“Why don’t we have the exact focus on palliative care, so anyone making the biggest decision of life can make an equitable, informed choice?”
It’s remiss of the Government, politicians and the Ministry of Health, he says.
Betty says New Zealand’s 5,500 GPs, specialist GPs, trainees and rural hospital doctors often provide palliative care to their patients free of charge.
That’s because there is no funding available for end-of-life care – a serious failing of the system, he says.
“Palliative care is so dependent on local funding, which is traditionally done by DHBs, but there’s a total lack of funding, resourcing and a national approach.”
This, coupled with a growing workload and an increasing complexity in clinical patient needs, adds pressure to palliative care practices.
“The question becomes – why don’t we have that exact same focus on palliative care,” Betty says.
The Assisted Dying Service Data and Report from 7 November 2021 to 30 September 2022 says only about 80 percent of those choosing assisted suicide or euthanasia have access to palliative care.
Betty cautions against this analysis.
“It doesn’t show perceptions of what is going on or the quality of care they are receiving,” he says.
The data’s effectiveness should be questioned when the Act is reviewed, he adds.
“Everyone is affected by death and dying. That is part of health. Good dying and having equitable choice is a fundamental part of the healthcare system we set up. It has to be given space and focus at this point.”
Source
Additional readingNews category: New Zealand, Palmerston.